The need in the osteoporosis “medicine cabinet” is for more bone formation medicines since Forteo is the only available medicine for targeting osteoblasts, the bone building cells. Research on how cells communicate with one another led to the identification of a complex system of messengers, called the Wnt signaling pathway, which plays a central role in regulating the growth and activity of osteoblasts. This discovery has opened the door for development of new compounds that target these messengers.
Sclerostin Decreases Bone-Building
One approach is try to block factors that decrease bone formation. A protein called sclerostin, produced by bone cells (osteocytes), is one of the messengers that sends the signal to apply the brakes in making new osteoblasts. The blocking of sclerostin allows the rate of bone formation to increase.
Osteoporosis Medicine Developed to Block Sclerostin
Amgen is testing a protein that neutralizes the effects of sclerostin. This unique osteoporosis medicine in development named romosozumab, (the compound was named AMG 785) is in clinical trials. Results of the 12-month phase 2 clinical trial was released online first in the New England Journal of Medicine as a featured article with an editorial. Lead author Dr. Micheal McClung from the Oregon Osteoporosis Center explains, “Unlike most of our current medicines that halt the progression of bone loss, romosozumab activates the bone forming cells and stimulates the production of new bone tissue. In studies of animals with osteoporosis, this therapy has normalized bone mass and bone strength.”
Romosozumab Results in Robust Bone Density Increases
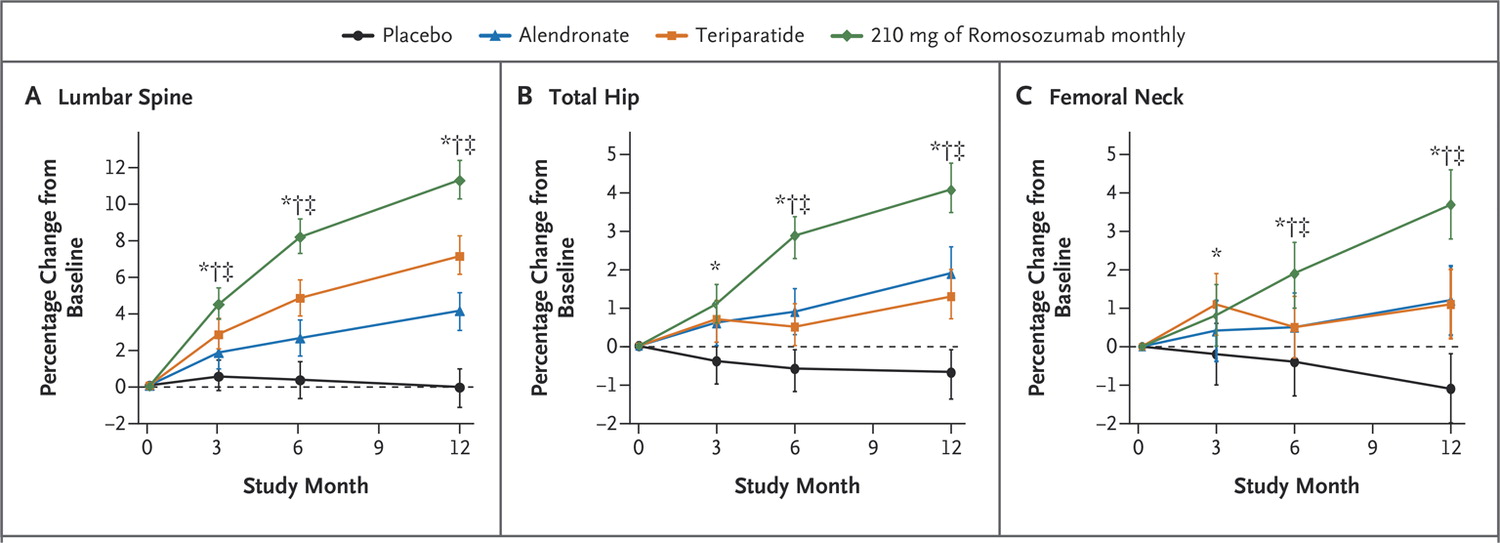
Phase 2 studies evaluate the safety and effectiveness in 100s of subjects. For research osteoporosis medicines, bone mineral density is the outcome. In this study, 5 different doses of Romosozumab were compared with placebo (no active medicine), daily Forteo (teriparatide) and once-a-week Fosamax (alendronate) in 419 women with postmenopausal osteoporosis. Romosozumab is given as a shot under the skin and depending on the dose was administered either monthly or every three months.
The figure below shows results at the end of 12 months. The group given the highest dose of romosozumab (210 mg every month) had the highest average bone mineral density (BMD) gains at the spine and regions of hip. The average BMD increase at the end of 12 months was 11.3% using the 210 mg monthly dose. These gains far exceeded the other two medicines and placebo groups. Daily teriparatide increased BMD at the lumbar spine by 7.1% and once-a-week alendronate by 4.1%.
Does Romosozumab Lower Fracture Risk?
Now the question is, how do those robust increases in bone density affect reducing the risk of fractures? Dr. McClung said, “Additional studies are underway to evaluate the effectiveness of romosozumab to reduce fracture risk in women with postmenopausal osteoporosis. If successful, romosozumab may be an important treatment option for patients with severe osteoporosis who are in need of skeletal restoration.”
The current medicines in development approach all new ways to treat osteoporosis. The future horizon appears bright for innovation in the area of osteoporosis medicines. For now, if you are at high risk of breaking bone talk with your health care practitioners about current options.
________________________________________
Diane L. Schneider, MD, MSc
Author, The Complete Book of Bone Health
Medical Editor, 4BoneHealth.org